 Most young babies spit up occasionally due to the immaturity of their digestive systems. In fact, more than 50 percent of babies aged three months or younger have at least one episode of reflux per day. This rate peaks at 67 percent at four months old. Often times, when a mother quits breastfeeding, her baby’s reflux worsens. This is hardly surprising, considering that the composition of formula makes it harder to digest.
Most young babies spit up occasionally due to the immaturity of their digestive systems. In fact, more than 50 percent of babies aged three months or younger have at least one episode of reflux per day. This rate peaks at 67 percent at four months old. Often times, when a mother quits breastfeeding, her baby’s reflux worsens. This is hardly surprising, considering that the composition of formula makes it harder to digest.
For a lot of babies, the discomfort of reflux is part and parcel of their mother’s decision to quit breastfeeding, and they simply have to endure it. However, the mother in this week’s story was determined that her baby would not suffer any longer. She embarked upon a painstaking journey, using frequent pumping and a supplemental nursing system, to reawaken her breasts.
“When I was pregnant I was very ambivalent about breastfeeding, I figured I’d give it a go and if it didn’t work out then that was okay, as formula was just as good. Most of my friends had experienced difficulties with breastfeeding. Some weren’t able to make it past the first few weeks; others managed to establish feeding but ran into problems at the 4 month mark. None of them wanted to move to formula at the time and I know they experienced a great deal of heartache over their failure. I vowed that I wouldn’t put myself through that.
From ambivalence to ambition

At the beginning of my 3rd trimester I had been diagnosed with gestational diabetes and advised by my midwife that at birth, should my baby have a low blood sugar, then he may need supplementation. Consequently, I had been instructed to hand express every night. I diligently did this, and after two weeks, I started to get a couple of ml of colostrum. Seeing my body actually producing milk, I began to think a little bit more seriously about breastfeeding.
Eventful birth
Fast forward to 38+6 weeks and after a long labour which ultimately ended in an emergency c –section Harrison was born, all 8lb 1.5oz of perfect at 7.41pm. It took a while for the medics to stitch me back up and I didn’t get to hold my baby until 9pm when they wheeled me back to the delivery suite.

Shell shocked

At this point the heavy cocktail of drugs I had taken began to wear off leaving me with terrible shakes and I nervously passed my baby to his dad as I was afraid I couldn’t hold him. The midwife led Dad through the motions of putting on a diaper and getting Harrison dressed while a nurse gave me a bed wash. I was, at this point, still completely shell shocked by the whole experience.
I had been awake 40 odd hours and truly did not think for myself, allowing myself to be guided by the hospital staff.
Clueless midwives
It was at least 3 hours before it was suggested that I should try and feed my newborn, at which point I excitedly said I wanted to breastfeed. The midwife told me she would ‘show me what a good latch felt like’. Great, I thought, I knew latch was really important. So she manhandled my breast into my son’s mouth and he latched straight on. The midwife asked if it hurt and I said that it did a little, so she unlatched him and we tried again. It still felt a bit uncomfortable so I told the midwife who unlatched him and we tried again. We did this several more times until my poor little boy got fed up and refused to latch at all. The midwife also got fed up and called someone else to ‘have a go’. The second midwife had little more success and eventually suggested I hand express so she could feed my colostrum to my son in a bottle.
Separation
Soon afterwards we were moved up to the ward where I had to say goodbye to my husband and was left alone with my baby. It was 2am, I had been awake for 45 hours straight and was beyond exhausted. I quickly began to drift off and then suddenly there was a wailing from the side of me. Being bed bound after the c-section and confused, I could do nothing but lie there, and a member of staff quickly popped her head round my curtain. “Shall I take him to the nursery?” she said, “Let you get some rest?” I think I nodded as she wheeled my baby off for the night and I quickly fell into a deep sleep.
Supplementation without consent

I woke with a start at 5 and pushed the buzzer to ask for my baby. The nursery nurse came in with him in her arms and told me it was good timing as he’d just been fed. At this point I didn’t realise what this meant, I was too busy staring in amazement at the tiny bundle in the cot next me. He still wouldn’t latch on properly and at some point we were given small bottles of formula to feed him. At every feed I called for help with breastfeeding, and they would spend ten minutes tugging at my breasts and pushing his little face into them until he latched on and then they’d walk away at which point he would almost immediately slip off and they would bring me more formula.
One helpful midwife bought me round a pump to see what I could get (quite a lot as it turns out) and suggested using expressed milk instead of formula where possible. Sadly she gave me no guidance on how to use the pump to build my supply so I expressed once or twice a day which provided enough milk for most of his feeds, and after that we used formula.
Supply dwindling
We were sent home at 3 days where, without any support, things went from bad to worse. Most attempts ended with both my baby and myself crying in frustration, followed by my husband feeding him with a bottle. I was still periodically expressing but the amount I was able to get was dwindling and he was for the most part formula fed.
At 3 weeks, my health visitor arrived and after I explained the difficulties we had been having, she suggested swaddling to prevent my son’s angry and frustrated fists from getting between him and my breast. At last, he latched, and he stayed there for 20 minutes!! I was over the moon. From then on I decided to try and get him back to breast and started offering the breast before every formula feed.
I was pretty sure my supply was almost gone at this point so was worried about starving him.
Although feeding did not suddenly become a dream, my son latched on more often than not and soon I started to reduce the number of bottles he was receiving. Tragically, no one had told me the mechanics of how milk production worked so I started with the day time breastfeeds and continued to formula feed overnight.
Public embarrassment
We had an element of success; however Harrison seemed to feed constantly. When at home he would feed for 4-5 hours straight, have a 20 minute nap, and then wake crying for more. I would literally not be able to move off of the sofa. If we went out, he would be fussy and irritable so I would hurry home to feed him.
I had a crippling fear of feeding in public. I was intensely embarrassed that my baby usually screamed at me when I offered him my breast, that I refused to feed where anyone could see us.
By 7 weeks I was exhausted and miserable and I needed a break, so I introduced a bottle of formula back into the day. That soon became a second bottle and then a third, and then before I knew it we were down to one breastfeed a day before just before bath time. That feed slowly got shorter and shorter and then at 15 weeks he refused my breast.
I had failed
I cried and I cried. Somewhere along the way breastfeeding had become critical to me and I had completely and utterly failed. The last 15 weeks had been difficult emotionally; I had been up and down, frequently crying at my inability to provide the best for my son, for failing him. My husband didn’t know what to do with me. He had really wanted me to breastfeed but could see the emotional toll it had taken on me and wanted me to feel better. It was hard on our relationship as I took a lot of my frustration out on him. Even though he tried to be supportive of me, I felt like he considered me a failure. We finally agreed that it was time to draw a line under the experience and move on. Except I couldn’t, and whenever he would let me I would latch Harrison on for a quick suckle, cherishing every moment.
A turning point
Then I read an article on Milk Matters (‘The hidden cause of feeding problems’) and so much of it resonated. One of my biggest concerns was that Harrison had developed reflux and was throwing up a lot, pretty much every time I picked him up we would end up covered in it. This had only become a problem as his diet had become more formula based and I felt quite strongly that breastmilk would resolve the issue. This was the point where I made my decision.
I was still able to produce a few beads of milk, and knew it was a demand and supply situation. So I decided to re-lactate. The support from my local Health Care professionals had been ridiculous to date (the best they could offer was spend more time at the breast, or ‘he must just be lazy’) so I didn’t seek help, I simply scoured the internet for success stories and planned my route of attack.
The relactation plan
I hired a hospital grade pump, stocked up on fenugreek capsules and asked my doctor for a prescription for Domperidone. I also got my husband on board with my crazy plan. He was initially nervous as he didn’t want me to get upset again if I couldn’t do it. However, he quickly recognised my determination and was 100% behind me, providing whatever help he could when he wasn’t at work. For instance, he would get up early with Harrison at the weekends to allow me to get an extra hours sleep and would occupy him while I was expressing.
I only told one other person in the early weeks about my relactation plan. I felt embarrassed and didn’t want people to know if I failed again. The friend I told was very supportive as she was struggling with her own demons at the time and understood my strong desire to succeed.

To start with, I expressed for 15 minutes every 2 hours around the clock. By the end of it I was exhausted and had managed to express just 10ml, but I was determined. This time nothing would stop me. I continued to express every 3 hours during the day and woke myself at 4am to express every night while my baby slept peacefully through. I also started offering the breast before every formula feed and at every other opportunity that presented itself. I offered my breast every time he cried, if he was bored, hungry, tired or just grumpy. I answered every issue with mummy’s milk.
In the early days the frequent pumping did tied me to the house. For 2 weeks I didn’t go out in order to focus on increasing my milk as much as possible. After that I relied on the pump less during the day and tried to feed direct from my breast instead. It was a long time though before I was able to go out of the house and not think about when I was going to express.
Tongue tied
During this time, I became convinced that Harrison was tongue tied and fought to get a diagnosis and treatment. I was lucky, in that the third professional I saw was a very knowledgeable infant feeding co-ordinator (IFC). She diagnosed a posterior tie then referred us for treatment. 2 weeks later the tie was cut. Much to my dismay it was not an instant improvement; instead it took several weeks for Harrison to learn to feed properly at the breast.
Supplemental Nursing System
During this time Harrison refused my breast for 4 days. I was devastated and ended up paying for a lactation consultant to come and see me. She knocked up a make shift Supplemental Nursing System (SNS) using a feeding tube and we tried it. It was amazing to watch Harrison feeding calmly and contentedly at the breast for the first time ever. I then bought a proper SNS. We used it for a couple of weeks. It was difficult to get Harrison latched on properly with the tube in the right place, and with my feeding in public issues there was no way I would have attempted it in public! It was however, a nifty little system and when at home it was worth the effort to use it.
Soon, my efforts were starting to pay dividends. Slowly but surely the amount I could express increased, and Harrison would feed for longer and longer at my breast, not requiring topping up. It wasn’t long before he was happy to latch on his own and we were able stop using the SNS.
Then one day I breastfeed Harrison as normal but he fell asleep on my breast before I could offer the formula top up. He slept for nearly 2 hours and when he woke he wasn’t looking for food. So we went for a walk… He didn’t have his next feed until nearly 3 hours later! So this was how it is meant to be? At this point the three daytime bottles were just 4oz, so from this day on we dropped one of the bottles completely and we are down to just 4 bottles a day.
Yet sadly, our difficulties were not over.
Baby-led weaning problems
Harrison started baby led weaning at 6 months and took to it enthusiastically. We soon noticed though that instead of swallowing food, a lot of it was ending up pushed into the roof of his mouth where it would stay until one of us fished it out. By this point he was on just two bottles a day, his bedtime bottle, and a small one in the late afternoon. I was struggling to phase out the afternoon bottle and couldn’t work out why. Then Harrison’s
weight gain halted. To reassure myself that I was producing enough milk I was getting him weighed every two weeks, and for three weeks his weight stayed the same. The hardest thing on this journey has been learning to have confidence in my body. When he’d been waking in the night I told myself it was the famous sleep regression . When he was grizzly in the evenings I told myself it was teething pain. And I nearly believed it. In an instant all the confidence I had been building was shattered. He was starving! That’s why he had been grizzly and waking in the night!
The health visitor started to push towards switching to puree weaning, but I was determined that I didn’t want to go down that route, so after turning to the internet again I decided that his tongue tie must have re-grown. This would explain the difficulty he had in moving food around his mouth, why my nipples had started to hurt again, and why it still felt like I wasn’t producing enough milk. A quick trip to the Infant Feeding Coordinator confirmed that this was the case, and an appointment was booked for our second division.
Then my father in law sadly passed away and we spent two days at the hospital with him, saying our final goodbyes. Harrison was looked after by other family who were given cartons of formula to feed him with as I had nothing else to give. When we picked him up before going home he was clearly very uncomfortable, grouchy and vomiting again. It was so obvious how much formula did not agree with him, so from that point onward we swore he would not have another drop of the stuff.
At 7 months, Harrison had his second tongue-tie division. On the very same day he swallowed his first ‘food’, the paper napkin my mother-in-law had given him to play with (don’t get me started!), and the evidence was for all to see in his diaper the next morning! We got rid of that afternoon bottle and were left with just the bedtime one to deal with.
Father’s reluctance to cease bottle-feeding
I was still having to express three times a day to get enough milk for the bedtime feed. It was hard work and a right pain! However, Daddy loved doing that bedtime feed, and so I found it difficult to take that from him. He enjoyed the one-to-one time with Harrison and enjoyed being able to put him to bed.
At around 10 months, Harrison caught a minor virus complete with a couple of nights of vomiting and high temps. He refused the bottle, preferring to feed from me instead. He was clearly comforted by nursing and my husband was relieved to know that he was staying hydrated. By that age, it was easy to see what a good relationship the two of them shared, so he quickly realised that he didn’t need to feed him as he had plenty of other ways to be involved.
From that moment onward we never looked back.
He is currently 17 months and still going strong. We’ve struggled through a couple of sleep regressions, a few bouts of cracked nipples, and a couple of blocked ducts but our nursing relationship is stronger than ever, and an integral part of our relationship. Once the tongue tie was dealt with, we quickly conquered our nursing in public demons and these days I am proud to openly nurse my baby.

It started to feel a bit lonely as my friends began to wean their babies onto formula, but I found new support in joining my local la leche league toddler group. Unfortunately, we still encountered some prejudice from my family, especially as Harrison has gotten older and they have found our nursing relationship more difficult to understand. It saddens me that they can’t celebrate my achievements with me, and instead ask me to hide myself away as though I am doing something shameful or indecent. My sister, in particular, is embarrassed by it and doesn’t like me to feed in front of her at all. Sadly, this has affected our relationship. I have given up quoting World Health Organization guidelines as they don’t consider that they apply to developed countries.

Alas, I won’t let that affect the nursing relationship I have with my son as I know that I am providing him with the very best nature can offer. I understand why some women choose to formula feed – I was nearly one of them. Yet despite almost becoming another statistic, I can hold my head high and know that I have done the very best that I could do.”
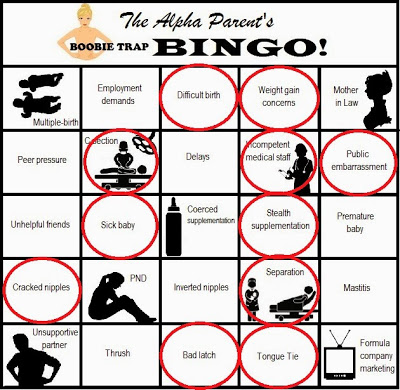
Get your own blank Bingo Card here.
Email me with your story to appear on Triumphant Tuesday!
 Most young babies spit up occasionally due to the immaturity of their digestive systems. In fact, more than 50 percent of babies aged three months or younger have at least one episode of reflux per day. This rate peaks at 67 percent at four months old. Often times, when a mother quits breastfeeding, her baby’s reflux worsens. This is hardly surprising, considering that the composition of formula makes it harder to digest.
Most young babies spit up occasionally due to the immaturity of their digestive systems. In fact, more than 50 percent of babies aged three months or younger have at least one episode of reflux per day. This rate peaks at 67 percent at four months old. Often times, when a mother quits breastfeeding, her baby’s reflux worsens. This is hardly surprising, considering that the composition of formula makes it harder to digest.

 At this point the heavy cocktail of drugs I had taken began to wear off leaving me with terrible shakes and I nervously passed my baby to his dad as I was afraid I couldn’t hold him. The midwife led Dad through the motions of putting on a diaper and getting Harrison dressed while a nurse gave me a bed wash. I was, at this point, still completely shell shocked by the whole experience. I had been awake 40 odd hours and truly did not think for myself, allowing myself to be guided by the hospital staff.
At this point the heavy cocktail of drugs I had taken began to wear off leaving me with terrible shakes and I nervously passed my baby to his dad as I was afraid I couldn’t hold him. The midwife led Dad through the motions of putting on a diaper and getting Harrison dressed while a nurse gave me a bed wash. I was, at this point, still completely shell shocked by the whole experience. I had been awake 40 odd hours and truly did not think for myself, allowing myself to be guided by the hospital staff.