 If a health professional administered a drug to your child that later left them with chronic health problems, they would be guilty of medical negligence. They may very well lose their job over it, and rightly so. However, this degree of justice is routinely denied to the most vulnerable of patients. Indeed, there is a loophole in patient protection, whereby health professionals can administer medication without consent and against the patient’s best interests. Yup, I’m talking about formula.
If a health professional administered a drug to your child that later left them with chronic health problems, they would be guilty of medical negligence. They may very well lose their job over it, and rightly so. However, this degree of justice is routinely denied to the most vulnerable of patients. Indeed, there is a loophole in patient protection, whereby health professionals can administer medication without consent and against the patient’s best interests. Yup, I’m talking about formula.
This is the heartbreaking story of baby Hermione who, when born prematurely, was given formula against her mother’s express wishes. She later went on to become very ill indeed.
“In March 2012 I gave birth to my daughter, Hermione, four weeks early and weighing 4lb and 8oz. I had planned a home birth and to breastfeed immediately but as my waters broke at 36 weeks I was induced in hospital. It was a fast labour and I was very sleepy and nauseous throughout.
Separation

As Hermione was early and very small she was swiftly moved up to Transitional Care Ward. I trusted that the healthcare professionals would support me to establish breastfeeding, naively believing everything I was told and didn’t have the evidence to back up any misgivings at the time.
I was taken up to the ward and saw her in an incubator in the nursery with a feeding tube and antibiotic cannula. I was then taken to my bed, where I stayed. After a brief sleep I awoke feeling utterly bereft and asked to see Hermione. She was wheeled through in her incubator.
Formula given without consent
At some point Hermione had already been given formula although I had not been consulted! I had made it clear I wanted to breastfeed on my birth plan and in my maternity notes. I felt completely violated! Yet, I wasn’t aware of my consent being required so felt powerless to complain. No one approached me to suggest initiating breastfeeding, I had to ask. I felt Hermione had been left too long without me; it was seven hours since I had given birth.
I then breastfed Hermione at around 5pm and she fed well. She breastfed regularly, especially on day two when she was then feeding every hour or so and no longer needed the incubator as her temperature had stabilised. I was tired but happy with her regular feeding as I knew she was stimulating my milk supply. All I needed was reassurance at this stage, yet I was told by hospital staff on several occasions that Hermione didn’t have a good latch. Yet I didn’t have sore nipples nor did I ever have to use lanolin. Hermione knew what she was doing even if everyone else didn’t.
Formula pushing
However, in the evening of day two, a nurse suggested I give her a top up of formula, why? Because Hermione was feeding so much. I was also told to limit her feeds to 20 mins and then give formula as apparently she “wasn’t getting any milk after then” and was using more energy than gaining. I was very annoyed and confused as I didn’t understand why she needed anything but my breast milk. I strongly rejected this and carried on breastfeeding on Hermione’s cue throughout the night. However the seed had been planted, ‘I didn’t have enough milk as my baby was feeding too much’.
That night Hermione fed for 4 hours without a break and a midwife, instead of supporting me, stated “this is what you have to do if you do not want baby to have a top up of formula.”
Did she have jaundice?

On day three I woke up engorged and was so relieved that my mature milk had arrived. Hermione was still breastfeeding well throughout the day, although my mum said that evening she looked jaundiced. Whilst being weighed I mentioned this to the nurse but was told Hermione didn’t have jaundice.
On day four Hermione was very sleepy while breastfeeding and at some point it was confirmed that she did indeed have jaundice. Due to the high level of bilirubin she needed phototherapy treatment and some of this time was spent away from me in the nursery. Obviously, this led to her breastfeeding less than she should.
Discouraged from public breastfeeding
On one occasion in the hospital nursery, Hermione became distressed after having her blood taken, so I started to breastfeed her. I remember looking out of the window at the sunshine. I felt elated and incredibly proud, good old oxytocin! Then a nurse said I should go to bed and feed Hermione in private, and I felt terrible, like I was committing a crime. If I’d needed privacy I wouldn’t have fed her there in the first place. I said I was ok feeding Hermione there and continued but then felt uncomfortable and never fed her away from my bed again throughout my stay in hospital. Looking back, I feel there’s the view that breastfeeding women make formula feeders feel guilty so they don’t want us to be seen. Out of sight, out of mind.
Hermione recovered from jaundice and although she lost almost 10% of her birth weight, she did regain some weight. I recall comments that she was still feeding for too long and don’t know if this unconscientiously made me curtail her feeds but it certainly didn’t give me any confidence.
By this point, Hermione was still somewhat sleepy and had difficulty staying awake whilst breastfeeding. Jaundice prevents babies feeding properly due to the tiredness. I was given a hand expression kit. It contained a small dish to express into, a cup to feed baby and an instruction leaflet. However I wasn’t told why I needed to express, so being naive, I didn’t. On day five I left hospital and was discharged under the care of outreach.
Fretful baby

Day six and seven were horrendous; Hermione was very unsettled, never seemed satisfied after breastfeeding and wouldn’t sleep except on me. On hindsight she was just having a growth spurt, but no one had explained this to me so I was left doubting my milk supply, again.
More formula without consent
On day seven her blood was taken and, as her jaundice had returned, we were readmitted into Transitional Care Ward. During this stay, Hermione received more phototherapy treatment and overcame the jaundice within a couple of days. I asked to be woken when she needed breastfeeding. On at least one occasion I was not woken and Hermione was given a full 2oz formula feed. It was the same nurse who had previously encouraged me to top up with formula at the end of day two. At no point was I ever told the importance of night feeds to stimulate early milk supply or the importance of breast milk to combat jaundice (it contains a specific protein that reduces bilirubin levels).
Using the breast pump as a supply gauge
One morning a nurse suggested that I use an electric breast pump after I’d breastfed Hermione. I only managed to express 5ml and was totally devastated when she informed me that I didn’t have enough milk to feed my baby. Again, this was wrong information as a baby is much more efficient in removing milk from the breast; therefore expressed milk volume does not necessarily represent supply. Expressing milk via a pump is a skill that has to be learned and some women can never trigger their let-down via a pump but can breastfeed their baby successfully. Furthermore, Hermione had just breastfed which would have reduced any available milk anyway!
Suicidal
After this incorrect revelation about my low milk levels I became very depressed and suicidal; all I wanted to do was to breastfeed my baby and to be supported. I now felt I had no purpose in life as I couldn’t breastfeed Hermione – utter devastation. It had never occurred to me that I wouldn’t be able to successfully breastfeed and it literally felt like part of me had died. This was a very real symptom due to the affect of the milk factory starting to shut down as the night top ups had reduced my supply. The feelings were very frightening as I had no control on the level of care I received despite begging for help to breastfeed. A mental health doctor diagnosed PND. I was put on domperidone medication to help increase my milk supply.
I remember asking a nurse for a breastfeeding specialist and was quite rudely informed that all staff on the ward had breastfeeding training. I had no idea of the existence of lactation consultants or any good websites for help. I do remember a very supportive nurse who advised me to express after every feed to increase my supply. She also suggested different breastfeeding positions and was generally encouraging. Unfortunately she wasn’t always on shift and I was at the mercy of other nurses most of the time.
More formula pushing

By day five I had been told I had to top up Hermione with a certain brand of formula after every feed as “she was starving”. This felt totally alien as I’d never even considered formula feeding. I was told “babies are fine on formula”. Even though I did not agree, I felt powerless to object. By this stage I was totally consumed with guilt that I’d failed my baby, that Hermione was starving because of my alleged inadequacies whilst also instinctively knowing that formula was wrong for her.
After most formula feeds Hermione was sick. Often full-feeds. A nurse said it was just normal positing but I now know it was more than that. It really upset me when she vomited as I knew she was also bringing up some of my milk too. She’d always want feeding again within the next hour. Yet, I was never given impartial information about potential health risks of formula feeding, and was pressured into giving it as opposed to someone helping me to establish breastfeeding.
I was also told personal stories by the hospital staff they couldn’t breastfeed as their baby wouldn’t latch on. Why they told me this, I have no idea. It wasn’t relevant to my situation as Hermione’s latch was always fine, she was just sleepy and had no energy reserves due to her tiny size.
Forced to go home
After the second five day stay in hospital I was discharged with a tub of formula. I certainly didn’t want to be discharged as I didn’t feel mentally ready and didn’t want to rely on formula feeding, yet felt this was provided as a quick fix. Had I been allowed to stay in hospital a few more days to allow breastfeeding to become established, it would have saved the NHS substantial costs in the long run. Go figure!
Incorrect formula preparation instructions
An outreach nurse verbally advised how to make up the formula: Boil the kettle and pour 60ml of the water into a bottle, leave it to cool for the next feed; then, when formula was required, add powder to the water, mix and warm ready to feed. These instructions are not only wrong but they could have resulted in tragedy, as formula powder is not sterile it must be added to freshly boiled water no cooler than 70oC. Yet I was told this method of making up formula was quicker when you had a hungry baby waiting for a feed. Nothing was mentioned of the risk to Hermione’s health. I was also informed to increase her formula top ups to 3oz after about a week, even though they knew I was aiming to exclusively breastfeed.
My feeding routine was thus: breastfeed first which took anything from 40 minutes to 1 hour, then top up with 2oz expressed breast milk if I had enough or formula, then express breast milk, then sterilise equipment ready for next feed. Hermione’s small size meant I found it very difficult to position her to maintain good attachment. After trial and error I found the rugby ball hold using a cushion was the most effective and was also the best for eye contact. She was feeding almost constantly and I was exhausted. I could see no end to the formula even though Hermione had cut the volume down to around 1oz, I still didn’t have the confidence or the know how to stop the top ups.
Dropping the formula top-ups

I visited my GP at four weeks and explained how I was feeling and how badly I wanted to exclusively breastfeed. He said “just go for it” as Hermione was now 5lb and much more content. I still had little confidence but decided to drop the daytime top ups and maintain nighttime top ups.
At week five Hermione had a seven hour growth spurt which lasted until early hours. The next morning, for the first time, I had the let-down feeling and finally knew I had enough milk. She slowly but surely gained weight and went from under 0.4 centile to 2nd centile by six months, at 14 months she had reached 50th centile. Hermione never vomited after she ceased consuming formula. She was also much more satisfied and would go then around 2 hours between feeds.
The impact of early formula feeding
Hermione has suffered health complaints since leaving hospital. At nine weeks she developed an inguinal hernia which was promptly and successfully repaired under general anaesthetic. She also developed eczema at four months, two months prior to commencing weaning onto solids. It began as small raised red dots, which started itching, went raw with her scratching, and then were weeping and bleeding. First she had them on her legs, then elbows, chest, back, arms, hands, shoulders, neck, hands and face. At its worse the only place not affected was her nappy area and feet.
Blood-stained sheets

Hermione was constantly scratching and she wore scratch-sleeves to bed. She’d get worse in the heat but had to stay covered to stop her scratching, it caused her considerable distress. Between 4 and 7 months she barely slept at night, she was in pain and her sheets were always blood stained. Her condition peaked just before 7 months and another mother suggested antihistamines. My doctor begrudgingly prescribed them and Hermione slept for the first night in 3 months!
Despite its severity, the cause of her eczema was never medically investigated. Instead, I was simply told to treat the symptoms. I tried Diprobase, Doublebase then found Aveeno cream worked best with a steroid for flare ups. Doublebase emollient bath additive and aveeno bath oil were useful for bathing instead of soap. When Hermione’s face got bad, our doctor suggested using Sudocrem, but this made itching worse. The next doctor we saw prescribed antibiotic steroid and oral antibiotics which didn’t really help. I then discovered Burts Bees petroleum free ointment. It worked wonders on her face so I used it on the rest of her too and it really helped to keep her moisturised and heal her broken skin.

Diet-wise, I decided to gave her goats milk, cheese and sheep’s yoghurt as I suspected that cows dairy was triggering her. The health visitor advised me against this so I switched to cow dairy products. Immediately, Hermione had diarrhoea and her eczema flared up for a month until I switched back to goats and sheep dairy.
As a knock on effect, Hermione has to avoid all foods containing nuts until three years old; she is more likely to be allergic to nuts as her allergy system has already been sensitised by the cow’s milk formula. Inguinal hernias in premature babies and eczema are conditions twice as likely to occur if the infant has received any artificial feed prior to 6 months. Therefore, had I been supported properly to exclusively breastfeed whilst in hospital it is more than likely both conditions would not have arisen, and Hermione would never have had to risk general anaesthetic at such a young age. I have also suffered postnatal depression as a result of the largely appalling, non-existent breastfeeding support.
Extended breastfeeding discouraged

It’s a shame I’ve lost faith in healthcare professionals. They should have been supporting a vulnerable and impressionable first-time mother. These struggles really marred my enjoyment of motherhood and still do to some extent, but I’m determined never to be undermined again and always stick to what I believe in.
Submitting the complaint
I decided to write letter of complaint, which was so difficult at first, but suddenly the hurt just flowed out of me. There was a lot of crying involved. I was able to find a policy or procedure that had been breached for every incident. I submitted my complaint to the chief executive of the hospital trust (NHS UK). I received a dismissive response so wrote another complaint. I then had a meeting with 2 hospital staff. Read all about my complaints process here.
Unfortunately, my husband has not been very supportive. He didn’t even read my complaint letters and has the opinion what’s done is done and I should stop going on about it. Yet this fight is important to me. I find it completely incomprehensible that some people don’t even try breastfeeding. To me, there is no choice. Breastfeeding is the only way to feed a baby.”
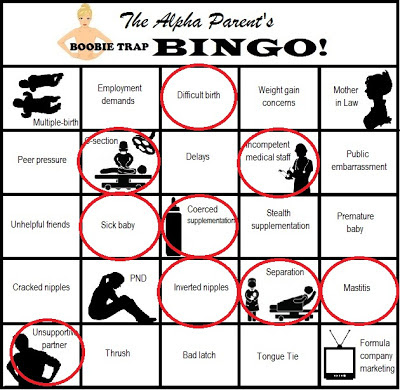
Get your own blank Bingo Card here.
Email me with your story to appear on Triumphant Tuesday!










