 Since pre-history, mothers in need of human milk have relied on other mothers in their family and community with milk to spare and share. According to the World Health Organization and UNICEF, the second-best feeding option, after breastfeeding, is breast milk expressed by a child’s own mother, followed by milk from a healthy wet-nurse or from a human-milk bank.
Since pre-history, mothers in need of human milk have relied on other mothers in their family and community with milk to spare and share. According to the World Health Organization and UNICEF, the second-best feeding option, after breastfeeding, is breast milk expressed by a child’s own mother, followed by milk from a healthy wet-nurse or from a human-milk bank.
Yet currently, demand by far outstrips supply, with not even a quarter being met. Furthermore, at $3–$6 an ounce, a week’s supply could cost as much as $750—something few parents can afford to pay even if banked milk were readily available.
“Intent on giving their babies what every baby needs most, mothers are bypassing milk banks and going directly to the supplier—other breastfeeding mothers with milk to spare” (Spangler 2011). So why the controversy behind wet nursing and milk sharing, and is it really more risky than formula feeding?
The milk-sharing debate

With the help of social media, mothers are increasingly aware that milk-sharing is a viable option for those who can’t breastfeed or obtain banked milk. Mothers of healthy babies who need milk are linking with other mothers willing to donate milk via chapters of two popular Facebook-based communities—Eats on Feets and Human Milk 4 Human Babies —operating in more than 50 countries.
These online communities allow donor mothers to share their milk, safely and ethically, in the belief that they and recipient mothers are capable of weighing the inherent benefits and risks and making informed decisions. This altruistic commerce-free exchange is grounded in the principle that all who are involved in milk sharing take full responsibility for their actions and subsequent outcomes.
However, the position staked out by some public health authorities, notably in Canada, France, Israel, and the U.S., including the Canadian Paediatric Society and the American Academy of Pediatrics is clear: Don’t do it!
Mothers Vs Medics: a jostle for control
Some in the health and medical establishment regard internet-based sharing as a threat both to their authority and to public health. They reject a system that operates outside their influence, that can’t be regulated, and where mothers alone exercise control. Some especially anxious observers go so far as to allege that mother-to-mother milk sharing undermines the ability of the few under-provisioned human-milk banks to meet the urgent needs of sick and preterm babies, by further reducing potential milk donations.
It should be noted that donor mothers have been breastfeeding their own children. With few exceptions, these mothers and their children are being followed closely by health care professionals with all that this implies for health status monitoring; and they are ready to discuss their lifestyle and disclose their medical records before sharing their milk. And yet controversially, health authorities are contending that mother-to-mother milk sharing is fundamentally riskier than feeding infant formula, and that it’s impossible for mothers, acting on their own, to minimize health risks.
Milk banks and poor management
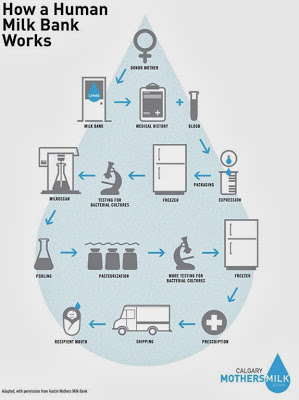
Milk banks function according to a strict medical model where regulations, rules, and protocol determine what is done, when, and for whom. Babies receiving banked donor milk are virtually always sick and hospitalized; healthy children seldom qualify for access to the limited amount of banked milk.
In addition, the screening criteria that milk banks typically apply disqualify many otherwise healthy women who might be willing to donate their milk. Exclusion criteria include previous residence in the UK (due to possible infection with mad cow disease), regular consumption of caffeinated beverages, a baby older than 6 months of age, and a small amount of available milk.
In contrast, milk sharing takes place in the community where interpersonal contact plays a significant role. Typically, the personalities and values of those involved are largely responsible for influencing decisions; the children concerned are healthy; and mothers are motivated by a heightened awareness of the importance of human milk for human babies and a desire to contribute to the common good. For some fascinating examples: click here to read the story of a woman that wet-nursed her niece; click here to read another story of a mother that fed her baby her friend’s milk.
Weighing and managing relative risk
There are risks associated with milk sharing just as there are with feeding babies formula. It is thus a question of weighing and managing relative risk, minimizing potential harm, and maximizing benefit. Rather than resisting and dismissing milk sharing, the constructive approach would be for health authorities and health care professionals to engage with mothers in ways that help make the practice as safe as possible, such as providing reliable information on donor screening, milk collection, storage, pasteurization, and feeding practices, and expediting voluntary sharing of medical records.
What the milk-sharing community advises:
The Four pillars to support the safe sharing of breast milk from Eats on Feets stress:
- Informed Choice—Mothers are responsible for understanding the options, including the risks and benefits, of all infant and child feeding methods.
- Donor Screening—Mothers can communicate with donors by asking questions about their health and lifestyle, and by requesting blood screening test results.
- Safe Handling—Mothers and donors should handle milk with clean hands and equipment and use proper storage methods.
- Home pasteurization—If in doubt, mothers can pasteurize milk at home: on the stovetop in order to inactivate HIV; or using a single bottle pasteurizer that performs the Holder method of pasteurization.

Wet-nursing and mother-to-mother human-milk sharing are here to stay. Though technology has transformed the practice, it remains fundamentally identical to what mothers of goodwill have been doing since pre-history on behalf of other mothers and their babies.
Not-for-profit human-milk banks and commerce-free mother-to-mother milk sharing can and should operate on parallel non-competitive tracks. They are complementary, not antagonistic. Indeed, there is significant untapped potential for both systems to play mutually supportive roles in pursuit of a single common objective—helping to ensure that no babies are denied their nutritional birthright.
 James Akre prepared this post for The Alpha Parent. As founder, chairman and CEO of the International Breastfeeding Support Collective, James focuses on the sociocultural dimension of the universal biological norm for feeding infants and young children, and on pathways for returning breastfeeding to the realm of the ho-hum ordinary everywhere. He is a member of the editorial board of the International Breastfeeding Journal and of the Scientific Advisory Committee of La Leche League France, and past member of the board of directors of the International Board of Lactation Consultant Examiners (IBLCE).
James Akre prepared this post for The Alpha Parent. As founder, chairman and CEO of the International Breastfeeding Support Collective, James focuses on the sociocultural dimension of the universal biological norm for feeding infants and young children, and on pathways for returning breastfeeding to the realm of the ho-hum ordinary everywhere. He is a member of the editorial board of the International Breastfeeding Journal and of the Scientific Advisory Committee of La Leche League France, and past member of the board of directors of the International Board of Lactation Consultant Examiners (IBLCE).










