All children suffer from illness at some stage. As a parent, I understand the anxiety and fear that you can feel when your child is unwell. When you are left with a child and a range of life-threatening illnesses your mind can start to play tricks. Also, during the early years in particular, the same symptoms can mean different things. Vomiting is a good example of this. To give you a better idea of what to look out for, I have created this comprehensive timeline detailing the most common illnesses throughout the entire span of childhood, from birth to teens. Fully referenced with up-to-date research, it aims to dispel some of the anxieties you may have, describes symptoms and explain when best to seek medical advice.
Jump to age…
| Newborn | 1 Week | 2 Weeks | 1 Month | 2 Months | 3 Months |
| 4 Months | 5 Months | 6 Months | 7 Months | 9 Months | 10 Months |
| 12 Months | 14 Months | 16 Months | 18 Months | 2 Years | 3 Years |
| 4 Years | 5 Years | 6 Years | 7 Years | 8 Years | 9 Years |
| 10 Years | 11 Years | 12 Years | 13 Years | 14 Years | 15 Years |
Newborn:
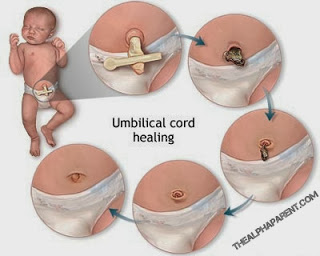 Umbilical Cord Problems: After a baby is born, the umbilical cord, which connected the baby to the placenta, is cut. In the majority of cases, the cord stump heals without problems but it can become infected or a collection of scar tissue (called a granuloma) may form. Until the cord stump has finally healed, infection can occur as the moist area around it can harbour potentially harmful bacteria. The exact cause of granuloma is not known but it may be more likely to occur if healing takes longer than usual. They usually disappear on their own, however if you suspect infection, see your doctor who may prescribe an antibiotic cream.
Umbilical Cord Problems: After a baby is born, the umbilical cord, which connected the baby to the placenta, is cut. In the majority of cases, the cord stump heals without problems but it can become infected or a collection of scar tissue (called a granuloma) may form. Until the cord stump has finally healed, infection can occur as the moist area around it can harbour potentially harmful bacteria. The exact cause of granuloma is not known but it may be more likely to occur if healing takes longer than usual. They usually disappear on their own, however if you suspect infection, see your doctor who may prescribe an antibiotic cream.- Bloodshot Eyes: This is a harmless condition that occurs when there is trauma to the eyeball – often in the form of broken blood vessels – during vaginal delivery. Like a skin bruise, the discolouration disappears in a few days and does not indicate there has been any damage to your baby’s eyes (Murkoff 2010).
- Erythema Neonatorum: It is common for newborns to develop this blotchy rash over the face and body. It is not known why it occurs, but it tends to get better within a few days without treatment (Kenny 2013).
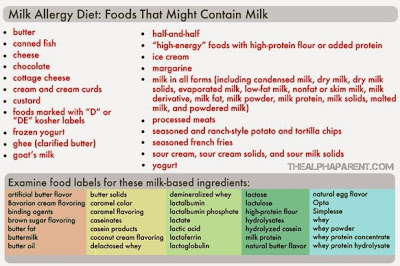
- Milk Allergy: Milk allergy is when your baby’s immune system reacts to proteins in milk. It is the most common childhood allergy, affecting between two per cent and seven per cent of babies. Babies who have eczema are more likely to suffer from it (Sicherer 2013). Your baby can take in milk protein through your breastmilk if you have drunk or eaten dairy produce, or she might react to cow’s milk-based formula milk. Babies can be allergic to casein in milk (the curd formed when milk turns sour), the whey (the watery part left when the curd is removed), or both. Symptoms include nausea, abdominal pain, bloating and diarrhoea. Breastfeeding mothers can alter their diet to address the symptoms (read two mothers’ stories here and here). Most children will have grown out of their milk allergy by the time they are three. Milk allergy is not to be confused with lactose intolerance which is when your baby has difficulty digesting the lactose, or the sugar, found in milk. This is much rarer than milk allergy.
- Bacterial Conjunctivitis: This is inflammation of the conjunctiva, the transparent membrane that covers the white part of the eye and the inner eyelids. Newborns sometimes develop bacterial conjunctivitis as a result of infection from the mother as they pass through the birth canal. Most cases of bacterial conjunctivitis are mild and do not require medical treatment as they get better within a few days. Several studies have shown that dispensing colostrum into the baby’s affected eye can speed up the recovery process (Singh et al 1982; Ibhanesebhor and Otobo 1996; Verd 2007; Baynham 2013).
- Cephalhaematoma: This is the medical term which describes a fluid-filled swelling on the head when occurs in some babies. During delivery, one of the blood vessels that lies on the outside of the skull bones ruptures due to the twisting forces. When it bleeds the blood is trapped between the bone and its strong outside covering, which leaves a prominent fluid-filled lump. This lasts anywhere from one month to six months and is nothing to worry about (Green 2010).

- Neonatal Jaundice: In jaundice, the skin and eyes have a yellowish tinge. It is common in newborns, effecting about 6 out of every 10 babies, and is not usually serious (NICE 2010). The yellow tinge is due to a build-up of bilirubin in the blood. Bilirubin is a waste product formed by the liver when red blood cells are broken down. Newborns have more red blood cells and the removal of bilirubin from the blood is slower than in adults as their livers are immature.
- Hydrocele: Newborn baby boys are sometimes born with a hydrocele. This is a collection of fluid within the scrotum, the sac that encloses the testes. Many hydroceles improve with time, and often no treatment is required. If your son’s hydrocele has not disappeared by the age of 1 or is very large and causing discomfort, it can be surgically removed (Kenny 2013).
- Hip Dislocation: One baby in about 250 is born with congenital hip dislocation (Valman 2013). In this condition, the head of the femur (thighbone) lies outside the socket of the pelvis or is unstable and is likely to slip out of position. Babies are screened for congenital hip dislocation soon after birth, and tests for the condition are included in routine check-ups during the first year of life. Congenital hip dislocation runs in families and is more common in girls than in boys (NHS 2006).
- Hypospadias: In this congenital abnormality, which affects boys, the opening of the urethra is located on the underside of the penis rather than at the tip. Hypospadias is detected during the routine physical examination that is done on all newborn babies. It is usually corrected by an operation that is performed before a boy is 2 years of age (Bupa 2012).
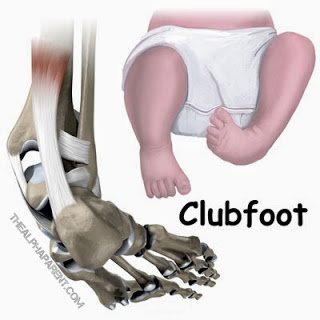 Clubfoot: This is a congenital deformity, also known as talipes, in which the foot is twisted out of shape or position. Clubfoot affects three times more male than female babies, and in half of all cases, both feet are affected (NHS 2013). Postural clubfoot is caused in the womb when the position of the baby’s foot forces it to be compressed. Unusually large babies are prone to this. Structural clubfoot is caused by an inherited abnormality of the bones in the foot. Structural clubfoot will require treatment.
Clubfoot: This is a congenital deformity, also known as talipes, in which the foot is twisted out of shape or position. Clubfoot affects three times more male than female babies, and in half of all cases, both feet are affected (NHS 2013). Postural clubfoot is caused in the womb when the position of the baby’s foot forces it to be compressed. Unusually large babies are prone to this. Structural clubfoot is caused by an inherited abnormality of the bones in the foot. Structural clubfoot will require treatment.- Hydrocele: This painless swelling of the scrotum occurs when fluid accumulates in the space around the testis. Hydroceles are very common in newborn babies, and they usually disappear without treatment by the age of 6 months (Chang et al 2010).
- Tongue-Tie: One in 10 babies are born with tongue-tie, a condition which can prevent them from breastfeeding effectively (Dillner 2011). Tongue-tie, also known as ankyloglossia, is a congenital oral anomaly which can decrease mobility of the tongue tip. It is caused by an unusually short, thick lingual frenulum, a membrane connecting the underside of the tongue to the floor of the mouth. Tongue-tie varies in degree of severity from mild cases characterized by mucous membrane bands to complete ankyloglossia whereby the tongue is tethered to the floor of the mouth. If feeding is affected, the tongue-tie needs to be divided. This involves cutting the short, tight piece of skin that connects the underside of the tongue to the floor of the mouth. It is a simple and painless procedure that usually resolves feeding problems straight away.
- Blue Baby: Babies may have mildly blue hands and feet, but this may not be a cause for concern. If their hands and feet turn a bit blue from cold, they should return to pink as soon as they are warm. Occasionally, the face, tongue, and lips may turn a little blue when the newborn is crying hard, but once he becomes calm, his color in these parts of the body should quickly return to normal. However, persistently blue skin coloring, especially with breathing difficulties and feeding difficulties, is a sign that the heart or lungs are not operating properly, and the baby is not getting enough oxygen in the blood. Immediate medical attention is essential










